Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- absence of hypovolaemia
- absence of hypervolaemia
- absence of signs of adrenal insufficiency or hypothyroidism
- nausea
- vomiting
- altered mental status
- headache
- seizure
- coma
Other diagnostic factors
- no history of recent diuretic use
Risk factors
- age >50 years
- pulmonary conditions (e.g., pneumonia)
- nursing home residence
- postoperative state
- malignancy
- medicine associated with SIADH induction
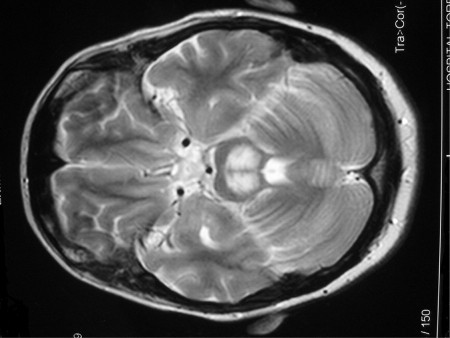
- central nervous system (CNS) disorder
- endurance exercise
Diagnostic investigations
1st investigations to order
- serum sodium
- serum osmolality
- serum urea
- urine osmolality
- urine sodium
Investigations to consider
- diagnostic trial with normal saline infusion
- serum uric acid
- fractional excretion of sodium
- fractional excretion of urea
- serum TSH
- serum cortisol level
- serum arginine vasopressin (AVP)
Treatment algorithm
severe symptoms
mild to moderate symptoms
asymptomatic with sodium ≥125 mmol/L (≥125 mEq/L)
persistence of chronic SIADH
Contributors
Authors
Megan Dixon, MD
Nephrologist
Arizona Kidney Disease and Hypertension Center
Phoenix
AZ
Disclosures
MD declares that she has no competing interests.
Howard Lien, MD, PhD
Professor Emeritus of Medicine
Division of Nephrology
University of Arizona
Tucson
AZ
Disclosures
HL is an author of a reference cited in this topic.
Peer reviewers
Judith H. Veis, MD
Associate Director
Nephrology
Washington Hospital Center
Washington
DC
Disclosures
JHV declares that she has no competing interests.
Laurie Solomon, MD, FRCP
Consultant Nephrologist
Renal Unit
Lancashire Teaching Hospitals
Fulwood
Preston
UK
Disclosures
LS declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Robertson GL. Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med. 2006 Jul;119(7 Suppl 1):S36-42. Abstract
Gross P. Clinical management of SIADH. Ther Adv Endocrinol Metab. 2012 Apr;3(2):61-73.Full text Abstract
Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Mar;170(3):G1-47.Full text Abstract
Ellison DH, Berl T. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007 May 17;356(20):2064-72. Abstract
Hoorn EJ, Zietse R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. 2017 May;28(5):1340-1349.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Pseudohyponatraemia
- Hypovolaemia
- Cerebral salt-wasting
More DifferentialsGuidelines
- Society for endocrinology endocrine emergency guidance: Emergency management of severe symptomatic hyponatraemia in adult patients
- Clinical practice guideline on diagnosis and treatment of hyponatraemia
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer