Summary
Definition
History and exam
Key diagnostic factors
- history of acute rheumatic fever (ARF) during childhood
- dyspnoea
- elevated jugular venous pressure with prominent a-wave
- low-frequency pre-systolic (diastolic) murmur at lower left sternal border
Other diagnostic factors
- age: 40 to 59 years
- exercise intolerance
- fatigue
- jugular pulsations
- abdominal swelling and discomfort
- oedema
- cyanosis or hypoxaemia
- atrial fibrillation
- hepatomegaly
- ascites, oedema, anasarca
- age: infancy or childhood
- episodic facial flushing, watery diarrhoea, or bronchoconstriction
- absent right ventricular lift or heave
- opening snap
- endocarditis stigmata (e.g., splinter haemorrhages, Osler nodes, Janeway lesions)
Risk factors
- group A streptococcal (GAS) pharyngitis
- metastatic carcinoid tumours
- artificial tricuspid valve
- intravenous drug use
- pacemaker/defibrillator leads crossing tricuspid valve orifice
- genetic predisposition and environmental factors
Diagnostic investigations
1st investigations to order
- ECG
- chest x-ray
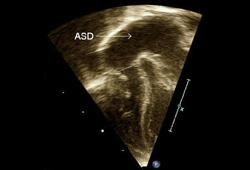
- 2D transthoracic echocardiogram
- Doppler transthoracic echocardiogram
- liver function tests
- blood biochemistry
- FBC
- blood cultures
- 24-hour urinary excretion of 5-hydroxy-indole acetic acid (5-HIAA)
Investigations to consider
- cardiac catheterisation
- cardiac MRI
- 3D transthoracic echocardiogram
Treatment algorithm
congenital
with carcinoid heart disease
with rheumatic fever sequelae
with infective endocarditis
Contributors
Authors
John R. Charpie, MD, PhD

Professor
Pediatrics and Communicable Diseases
Division Director
Pediatric Cardiology
Medical Director
Pediatric Cardiothoracic ICU
University of Michigan Congenital Heart Center
Ann Arbor
MI
Disclosures
JRC declares that he has no competing interests.
Jeffrey D. Zampi, MD

Associate Professor
Pediatrics and Communicable Diseases
Director, Interventional Pediatric Cardiology
University of Michigan Congenital Heart Center
Ann Arbor
MI
Disclosures
JDZ is and has been a consultant for Medtronic and Abbott.
Acknowledgements
Dr John R. Charpie and Dr Jeffrey D. Zampi would like to gratefully acknowledge Dr Martin L. Bocks, a previous contributor to this topic.
Disclosures
MLB declares that he has no competing interests.
Peer reviewers
Lokesh Tejwani, MD, FACC
Assistant Professor of Clinical Medicine
University of Missouri Hospitals and Clinics
Harry S. Truman VA Hospital
Columbia
MO
Disclosures
LT declares that he has no competing interests.
John Coltart, MD, FRCP, FACC, FESC, MRCS
Consultant Cardiologist
Cardio-thoracic Unit
Guy's and St Thomas' Hospital
London
UK
Disclosures
JC declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Roguin A, Rinkevich D, Milo S, et al. Long-term follow-up of patients with severe rheumatic tricuspid stenosis. Am Heart J. 1998 Jul;136(1):103-8. Abstract
World Health Organization. Rheumatic fever and rheumatic heart disease. Technical Report Series 923. Feb 2004 [internet publication].Full text
Baumgartner H, Hung J, Bermejo J, et al; American Society of Echocardiography, European Association of Echocardiography. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009 Jan;22(1):1-23. Abstract
Killip J 3rd, Lukas DS. Tricuspid stenosis physiologic criteria for diagnosis and hemodynamic abnormalities. Circulation. 1957 Jul;16(1):3-13. Abstract
Fawzy ME, Mercer EN, Dunn B, et al. Doppler echocardiography in the evaluation of tricuspid stenosis. Eur Heart J. 1989 Nov;10(11):985-90. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Cardiac tumours
- Systemic lupus erythematosus (SLE)
- Constrictive pericarditis (CP)
More DifferentialsGuidelines
- 2020 ACC/AHA guideline for the management of patients with valvular heart disease
- Heart valve disease presenting in adults: investigation and management
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer